One of the most turbulent wars that the science world has known in recent decades has just come to an end. It did not concern the war over global warming nor cancer or the obesity epidemic; this was a bitter and expensive war over credit between the wealthiest scientists and research institutions in the world.
The development of the CRISPR – Cas9 (Clustered Regularly Interspaced Short Palindromic Repeats) technology which enables scientists, with the help of an enzyme borrowed from the bacteria and virus world, to accurately edit sections of DNA quickly, and most importantly – cheaply. On one side of the arena were two biochemists, Jennifer Doudna and Emmanuelle Charpentier, from the University of California, Berkeley and Max Planck in Berlin (respectively), who published a study in 2012 in which they succeeded in performing the first cut of bacterial DNA using the “in vitro” system, that is, outside of the bacterium.
The prestigious institutions and the well-regarded researchers hurried to register a patent for the discovery, but less than a year later, in 2013, the young researcher Feng Zhang, an American who immigrated to the US from China at the age of 11, and is considered a scientific prodigy, published a study of his own. The researcher, from the Broad Institute of Harvard and MIT Universities, demonstrated the use of CRISPR for the first time for cutting DNA in mammalian and plant cells, and this study was also submitted to the patent registry.
This month, after many long years of costly legal battles in which tens of millions of dollars were invested, the United States Court of Appeal decided that both of the two camps would be granted rights to the patent, with the Berkeley-Berlin group granted the use of the revolutionary technology in any environment, while the Harvard-MIT group will benefit from being entitled to apply it to mammalian and plant cells.

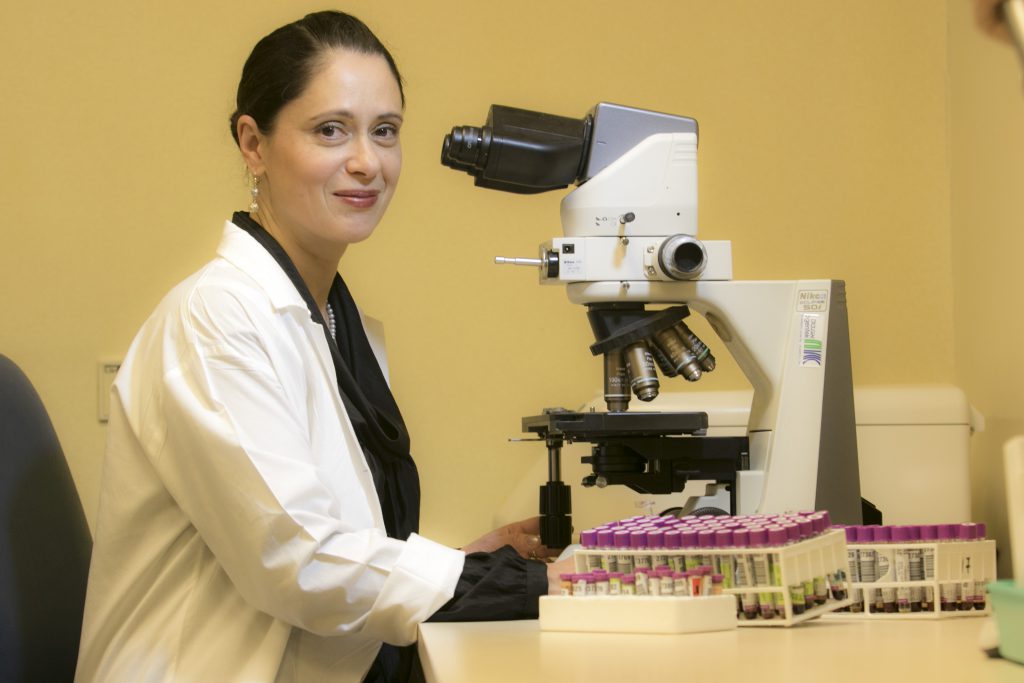
“The breakthrough here is the ability to take this mechanism, which is known in the context of bacteria that are able to protect against viruses, and to adapt it to human cells”, explains Professor Lena Basel Salmon, director of the Raphael Recanati Genetic Institute at Beilinson and Schneider hospitals and lecturer in pediatric medicine and genetics at Tel Aviv University. “We were actually inspired by them to create an RNA molecule that identifies a specific area in the DNA sequence, reaches it and knows how to cut it with the Cas9 enzyme which is attached to the RNA molecule. As its natural response to that kind of injury, the cell will correct itself, and this time with the correct DNA sequence, which will be presented to it by an additional molecule which will be injected into the cell. On the other hand, there is also the possibility of ‘spoiling’ during the repair of the natural gene and, in fact, “silencing” it – it is effective in treating diseases where the genetic problem is that a particular gene ‘works too much’”.
So why did the scientists exchange their lab coats for battle armor? Because the technological revolution in the microscopic world of the cell, just like with high-tech and computers, comes with lots of money and prestige. According to Professor Basel, there is no doubt that the use of this development will enter into the field of practical application in the field, and that the discoveries will win the Nobel Prize for the scientists behind them.
A rare price
This kind of discovery is a real revolution in how we are able to deal with a vast variety of diseases. “Use of CRISPR, right now is in the clinical trial stage, is presently focusing on treating immune system and blood diseases such as hemophilia and sickle-cell anemia, because it is relatively easy to remove the relevant cells, repair them and return them to the body”, Basel explains.
But the potential of genetic disease treatments is enormous. It can be divided into four levels: gene therapy in its simplest form focuses on the DNA or RNA level; this comes along with effects at the protein level (ie. the gene product) and the cell level. “It is possible to repair an injury at the individual mutation level, which will solve the problems of a few individual patients. On the other hand, it is also possible to repair damage on the level of the entire gene function or at the protein level, which will be suitable for a much broader patient population”.
A tremendous research and application effort in the field of gene therapy is currently focused on rare diseases. The reason is simple – rare diseases are typically caused by individual genes, while common diseases are caused or affected by dozens and sometimes hundreds of genes working together. “It’s like a puzzle of 100 pieces that need to be integrated with one another in order to create a final product”, Professor Basel explains. “A rare disease, on the other hand, ends with one gene. That is why treatment at the genetic level is more realistic with these cases”.
A slightly different form of gene therapy than the CRISPR, which is now on the agenda for many companies in the field, focuses on viruses and their ability to duplicate. The object is “to take a virus, attach a gene that the patient is missing or for whom it is not functioning well, insert this virus into the relevant organ, and there it will replicate itself while also replicating the gene attached to it”. Of course, these are viruses for which the ability to cause disease has been neutralized.
Scientifically, this kind of treatment is accompanied by a series of challenges. How should they deal with genes of different sizes? How can they cause a virus to multiply over time in order to provide longterm treatment? With the help of different types of viruses, today’s research is trying to manage these kinds of challenges, and have already logged real successes. Take, for instance, an innovative treatment for a rare type of retinal injury that causes blindness, developed by the American company Spark Therapeutics, which was the first gene therapy ever approved by the FDA, about a year ago.
Searching for a model
The scientific breakthroughs are not slow in coming, and many dozens of companies today are active in the industry, competing for the next gene therapy. However, the real challenge that they face is not science, but business. Spark’s treatment, which was supposed to kick off the revolution, is based on a sluggish market. Why? Because it costs the average patient (or his insurance company) about 850,000 dollars; and it is a market with very few patients. In 2012, the Dutch UniQure was the first company in history to receive regulatory approval to market gene therapy (it received approval in Europe, from the European Medicines Agency, the EMA). Only four years later they were forced to stop marketing the drug that they had developed – Glybera, which very effectively managed a disease called LPLD, which leads to the accumulation of fat in the bloodstream. It’s hard to blame them when the treatment was priced at $1 million for a single patient and the entire European market has only about 700 potential patients.
A study carried out by Harvard University estimates that by 2022, the FDA will have approved around 35 additional gene therapies. If no new business models are found to market them, their end may resemble that of Glybera. Spark does not intend to get to that point, and has recently developed a new business model of payment for just those treatments that succeeded (which minimizes the risk for insurance companies) and through payment plans. This is the first step towards what seems to be a need for a new health economy.
Knowing the way
One of the biggest questions impacting the effectiveness of gene therapy is “where?” In dealing with an organ such as the liver, it is relatively easy to inject it deliberately; but with diseases that affect multiple organs, or more sensitive organs, the medical challenge is considerable. In the brain, for example, an external vector that is injected will have to cross the blood-brain barrier (that is, to cross from the bloodstream into the fluid in which our brain sits), and such passage is very problematic. This is a challenge that needs to be circumvented when dreaming up a genetic therapy for Alzheimer’s, for example.
Although it is not a clearly gene-based disease, and therefore it is unlikely that it will be possible to “repair” anything that will prevent the development through gene therapy, it may be possible to neutralize its effects with a kind of bypass route. “At least conceptually”, Professor Basel allows herself a moment to contemplate the vision offered by scientific theory, “one can think of it as reprogramming some of our cells by changing genes. Maybe in the future we can turn those glia cells (whose name derives from the Latin word for glue), which are cells that are located around the neurons, into active neuronal cells. If you found a way to do that, you could create new neurons to replace the ones that died and, in fact, also treat diseases like Alzheimer’s or ALS”. Some companies in particular are already working in this field and are conducting lab experiments on animals. Others, such as the Israeli-American Orgenesis for example, which is in the development stages, is attempting to transform liver cells into insulin-producing cells and to transplant functional tissues composed of these cells back into the patient’s body as a diabetes treatment.
Another question that arises when discussing gene therapy is “how?” That is, is the strategy the repair of a specific gene mutation, such that it will be able to return to functioning properly, or rather disrupting the function of a gene (blocking the synthesis pathway of a particular protein, for example)? Such an action could be more universal in nature and not necessarily focused on a very specific repair. “Sometimes, when we make part of the DNA not express itself, we can actually improve the patient’s condition,” Professor Bassel explains. “For example, Duchenne muscular dystrophy can be very harsh, if we have a deficiency in a particular part of the relevant gene. But if we increase this deficiency, the patient’s condition will actually improve because protein segments will fuse, and an active molecule will be created, if only partially”.
At the same time, the research focuses on the repair of specific changes. “Every disease has its own particularities”, explains Basel“. In certain diseases of the bloodstream, such as sickle cell anemia, the genetic change is identical for the entire population of the world, so there is a point in the extensive scientific effort invested in this field.”
Timeline: Innovative Genetic Medicine
1960s: scientists discover the enzyme which enables the cutting and reconnecting of DNA sequences in test tubes
1970s: scientists successfully introduce new genes into animals through viruses
1990: the first successful treatment of a four-year-old girl with SCID, by replacing a damaged gene with an intact one
2012: the European Medicines Agency (EMA) approves the first gene therapy – Glybera – that deals with the hereditary disease LPLD
2012-2013: for the first time, scientists discover ways to use CRISPR technology, borrowed from bacteria, to cut genes at an exact location through use of the enzyme Cas9
2016: the European authorities approve the second gene therapy ever, Strimvelis, which treats a kind of SCID
2017: Spark Therapeutics receives the first ever approval in history for gene therapy in the USA; treatment of an advanced form of blindness
Translation by Zoe Jordan




